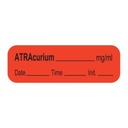
LABEL for Atracurium, roll
Valid Article
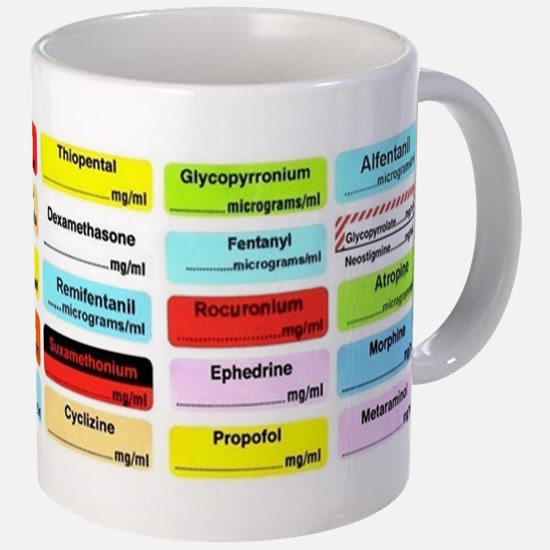
LABEL for injectable drugs
Definition
Pre-printed adhesive label (according to ISO standards) for the correct identification of injectable medicines in the perioperative area, designed to reduce medication errors.
Specifications
Quality Standards Comment
ASTM D4267 - 07(2015): Standard Specification for Labels for Small-Volume (100 mL or Less) Parenteral Drug Containers.
ISO 26825:2020: Anaesthetic and respiratory equipment -- User-applied labels for syringes containing drugs used during anaesthesia -- Colours, design and performance.
Technical specifications
- Adhesive:
- The label must be self-adhesive
- Label separation:
- If labels are supplied in tape form, the cutting area between labels must be perforated or clearly marked.
- Backing material:
- If backing material is used, labels must be easily detachable from both the backing and adjacent labels.
- Writeable surface:
- The label material should allow additional information (e.g. drug concentration) to be written using a ball-point pen without smudging or blurring.
- Background colour and patterns:
- Background colours and patterns should comply with ISO specifications. The background colour must not impair the legibility of additional information written with a black ball-point pen.
- Drugs with opposite actions (including antagonists):
- use 1 mm wide diagonal stripes of the designated colour, alternating with 1 mm wide white stripes.
- At least the top 20 % of the label must feature these diagonal stripes.
- The top of the drug name must be separated from the diagonal stripes by at least 0.5 mm.
- Label dimension:
- Length: 25 mm to 40 mm
- Width: 10 mm to 15 mm
- Drug name typography:
- The height of the letters should be as large as possible, but not less than 2.5 mm.
- Plain sans-serif style (bold or semi-bold style), with clear spacing and proportion:
- lowercase letters with an initial uppercase (e.g. Midazolam)
- "Tall Man" lettering: lowercase letters with distinctive parts uppercase (e.g. fentaNYL)
- do not use all-uppercase lettering
- Layout guidelines:
- Except for drugs with opposite actions (including antagonists), the drug name should be printed in the upper half of the label to leave space to below fro strength information.
- All letters should be black, except in the following cases:
- suxamethonium and adrenaline must be printed in inverted bold white letters on a black bar spanning the upper half of the label. The rest of the label should display the appropriate coloured background.
- Concentration unit:
- May be pre-printed in the bottom-right corner of the label.
Note on Tall Man Lettering:
Due to the lack of standardisation of Tall Man lettering, it is recommended to follow recognised sources such as:
- FDA and IMSP (Institute for Safe Medication Practice): DOPamine, diazePAM, ePHEDrine and fentaNYL.
- Additional examples proposed by the CCWG: KETAmine, PROPofol, THIOpental, MIDAzolam, ATRAcurium, VECUronium, SUXAmenthonium (= succinylcholine), NEOstigmine, MORPhine, NALoxone, LIDOcaine, BUPIvacaine, ONDAnsetron, DEXAmethasone, aTROPine, PHENylephrine, ADREnaline, ANTIbiotic, OXYTocin.
Packaging & Labelling
Presentation in rolls. The number of labels per roll varies depending on the manufacturer: 400 to 1000 labels per roll.
The quantity to be ordered should be based on the number of rolls, not the total number of individual labels.
Some label rolls are presented in dispenser boxes. Certain manufacturers offer different models of label dispensers that can hold between 6 and 24 rolls.
To be Ordered Separately
Dispensor for syringe labels
Instructions for use
Storage
- Below 25°C - Protect from sunlight - Protect from humidity
- Keep labels in their protective packaging, away from dust until use.
MSF requirements
The purpose of these recommendations is to standardise labelling and facilitate the identification and differentiation of syringes and containers (bags, bottles, etc.) containing injectable medicines used in anaesthesia, in order to reduce the risk of medication errors in MSF projects.
These recommendations apply to operating theatres, recovery rooms, and anaesthesia or sedation areas outside the operating rooms in MSF projects.

![[DINJATRB2A-] ATRACURIUM besilate, 10mg/ml, 2.5ml, amp.](/web/image/product.template/571693/image_256/%5BDINJATRB2A-%5D%20ATRACURIUM%20besilate%2C%2010mg-ml%2C%202.5ml%2C%20amp.?unique=e49fc79)